Background and Diagnosis
Periodontal disease is a bacteria-related inflammatory disease of the gums, the cementum that covers the root, the periodontal ligament and the bone around the tooth. Periodontitis can lead to pain, smell and tooth loss; in addition, it has been linked to heart disease and several other dangerous systemic conditions.
To determine if you have periodontal disease, and the extent of its progression, we begin by using a dental instrument to measure the pocket depth between your gums and your teeth. Ideally, the pocket depths around the teeth will range between 1 and 3 millimeters (mm). Gingivitis will appear as swollen gums and reveal pockets up to 4 mm. Both can be remedied by a simple cleaning.
Periodontitis, however, will be accompanied by red, irritated, bleeding, sometimes sore gums or pus and pockets deeper than 5 mm. Xrays of periodontitis will often show hardened calculus around the teeth and may even show the bone loss itself. A more detailed cleaning is in order to address periodontitis.
A great deal more is learned about the specific causes and circumstances surrounding each patient’s condition during the treatment itself.
Treatment
To treat periodontitis, we remove the deposits of calcified plaque called calculus or tartar and any other bacterial toxins which become ingrained under the gumline and into the root surfaces. The process, known as scaling and root planing (“SRP”), utilizes ultrasonic and hand scaling instruments, ideally while the patient is under local anesthesia. Just a few areas are focused on at a time until a “deep” cleaning is achieved.
In addition, the placement of a medicine called Arestin into pockets 5mm or greater is recommended. This medicine eliminates the harmful bacteria for 45 days following SRP.
Immediately following SRPs, it is recommended that patients use a Chlorhexidine Rinse, an antibacterial mouthwash that helps to control and kill the bacteria in your mouth that cause gum disease. We recommend that you rinse with chlorhexidine after brushing your teeth for one week following SRP and after future dental visits.
Existing bone loss related to periodontitis will not return with SRP. But, SRP’s and a few changes to your routine cleaning protocol described below will help you keep your teeth for life.
After Care
Instead of a simple cleaning (“Adult Prophylaxis”), Periodontal Maintenance describes the type of routine office cleanings following SRP. It is considered a basic service by insurance.
Periodontal Maintenance removes plaque and tartar from above and below the gumline, down the length of each tooth to where the root, gum and bone meet. Rough areas of the roots are maintained smooth, pocket depths are carefully monitored, and inflamed pockets are irrigated with antibacterial medicines if necessary.
After SRP treatment, most patients choose to have their teeth cleaned every 3 or 4 months to match the complexity of their dental condition that led to the periodontitis in the first place. These factors include their natural plaque and tartar accumulation, bleeding, inflammation, pocket stability, the quality of their anticipated home care and their overall health risk factors.
Lastly, with a few meaningful changes to your at-home cleaning routine, periodontitis can be kept under control. Brushing for two full minutes twice daily with an Philips Sonicare toothbrush and flossing once a day is usually adequate. For difficult areas, christmas tree brushes (“proxy brushes”), enlarged floss (“super floss”) and Philips Airfloss are excellent aids. Consistent behavior change is the most important element in maintaining long term periodontal health. Smoking has also been shown to contribute to periodontitis.
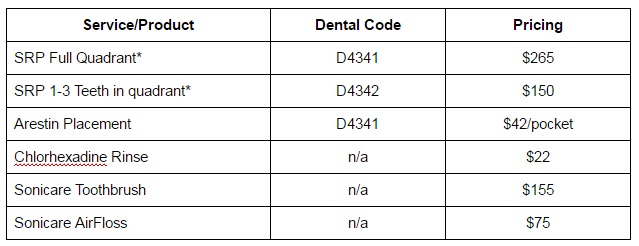
Related Pricing
*Dental insurance plans will often cover all or part of these costs.
More Information
Have more questions? We want you to have a complete understanding of your oral health and how to best maintain or improve it. You may want to do some research on your own. Here are several internet search terms to help you get started:
- Periodontitis
- Gum disease
- Link of periodontitis to systemic health
- Scaling and Root Planing
- Periodontal Maintenance
- Arestin
- Chlorhexidine rinse
- Philips Sonicare
- Philips Airfloss
- Scaling and root planing and insurance
- Reasons for tooth loss
- Cause of bleeding gums
- Risk of deep periodontal pockets
- Periodontal surgery
- Options for missing teeth
- Dentures
- Implants
- Implants with periodontitis